Stop the Inflammation. Preserve Your Vision.
Uveitis is an inflammatory eye condition that can cause lasting damage without the right diagnosis and treatment. Our board-certified ophthalmologist, Dr. Sandip Suresh, specializes in the diagnoses and treatment of all forms of uveitis—whether it’s acute, chronic, or linked to a systemic condition.
“Dr. Suresh is simply the best. He has an amazing team and you will not be disappointed in any aspect of your treatment. Over many years, I had numerous issues go undiagnosed or misdiagnosed. That is, until I found Dr. Suresh.
”
- Eye Care Patient
What Is Uveitis?
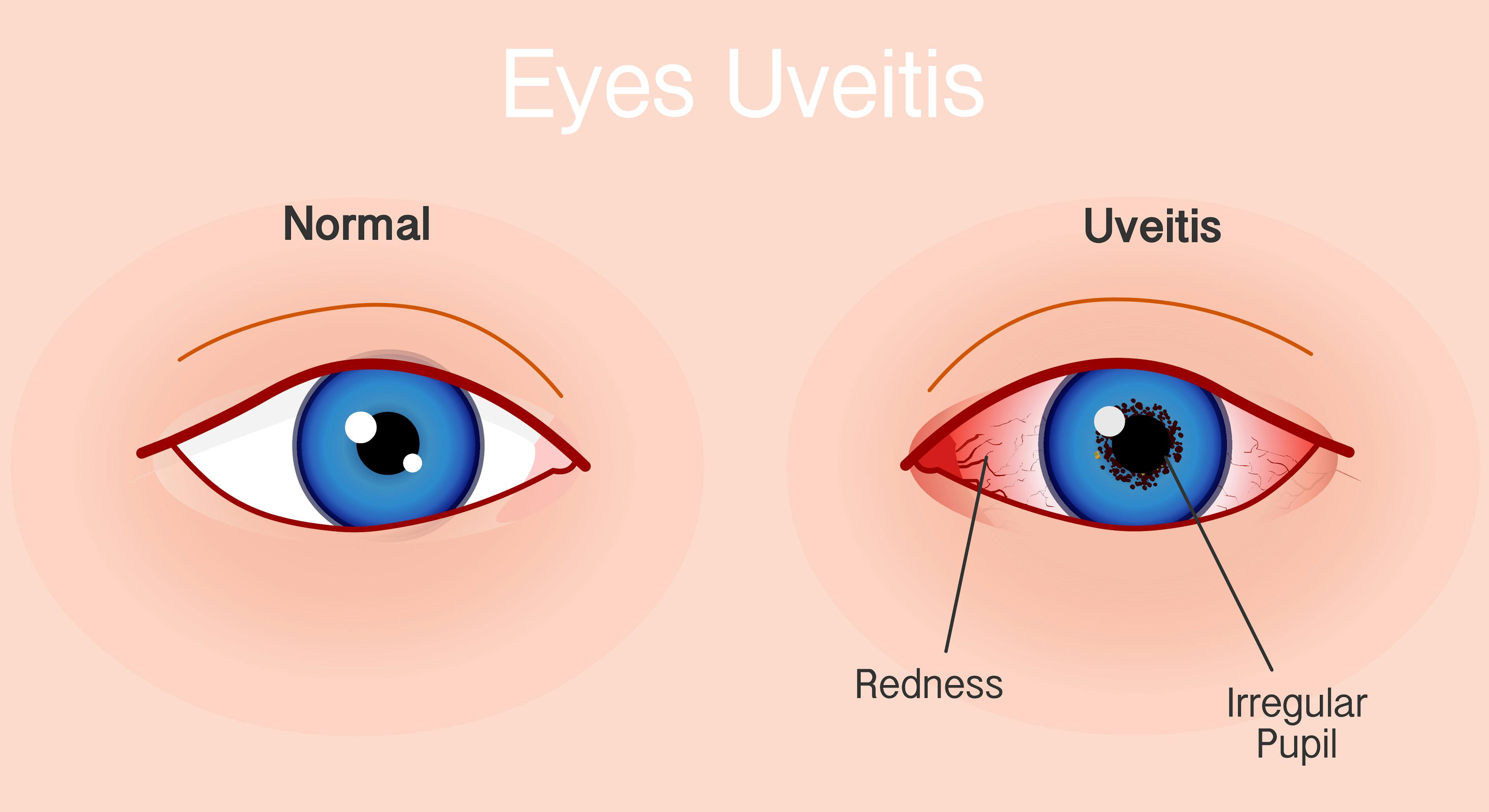
Uveitis is inflammation inside the eye. It can affect the iris, ciliary body, and choroid (the uvea), as well as nearby structures like the retina or optic nerve. Symptoms can develop gradually or appear suddenly, and the severity can vary from mild discomfort to vision-threatening complications.
Common Uveitis Symptoms Include:
- Blurry vision
- Eye redness
- Light sensitivity
- Eye pain
- Floaters or spots in vision
Uveitis is often caused by an underlying autoimmune disease, infection, or trauma. In many cases, no specific cause is found. Prompt, thorough evaluation is critical for guiding treatment and protecting long-term vision.
Our Diagnostic Process
We begin with a detailed eye exam and a complete review of your health history. Depending on the type and location of inflammation, we may recommend:
- Optical coherence tomography (OCT)
- Fluorescein angiography
- Ultrasound imaging
- Bloodwork to check for systemic causes
- Referrals for systemic evaluations when appropriate
Our ophthalmology team uses these tools to classify your uveitis (anterior, intermediate, posterior, or panuveitis) and determine the best next steps.
Treatment Options for Uveitis
Uveitis treatment depends on the cause, severity, and location of inflammation. We offer a full range of medical treatments, including:
- Prescription eye drops (typically corticosteroids)
- Oral anti-inflammatory medications
- Steroid injections
- Immunosuppressive therapies
- Biologic medications for autoimmune or chronic cases
- Surgical interventions
Our team monitors response closely and adjusts the plan to keep inflammation under control while minimizing side effects. For patients with recurring or long-term uveitis, we focus on reducing flare-ups and protecting the structures of the eye over time.
Coordinated, Team-Based Eye Care
Our approach to managing uveitis is collaborative and comprehensive. Your ophthalmologist leads your evaluation and treatment, and we work closely with rheumatologists, primary care physicians, and other specialists whenever uveitis may be linked to an underlying condition.
You’ll receive a clear care plan, continuity across providers, and long-term support from a team that understands the complexity of your diagnosis.
What to Expect at Your Appointment
- Comprehensive Eye Exam
We review your symptoms, medical history, and previous records if available. - Specialized Imaging
Tests such as OCT or angiography help us detect inflammation not visible during a standard exam. - Treatment Plan Discussion
We explain the type of uveitis you have, potential causes, and short- and long-term treatment options. - Start of Therapy
Initial treatment often begins the same day. You’ll receive prescriptions and instructions tailored to your condition. - Ongoing Monitoring
We schedule regular visits to monitor inflammation, track vision changes, and make medication adjustments as needed.
Why CLS Health for Uveitis?
- Experienced team of ophthalmology team trained in ocular inflammatory disease
- Advanced diagnostics to guide accurate treatment
- Full range of therapies for short-term control and long-term management
- Coordination with systemic care providers for whole-patient care
- Convenient appointments in Webster–Clear Lake
Get the Expert Support Your Eyes Deserve
Uveitis requires expert diagnosis and a treatment plan that evolves with your condition. At CLS Health Eye Center, we provide the care, coordination, and clinical attention you need to manage inflammation and protect your vision.
FAQs
Uveitis is inflammation inside the eye that affects the uvea—the middle layer made up of the iris, ciliary body, and choroid. It can also impact nearby structures like the retina or optic nerve. Uveitis can cause eye pain, light sensitivity, blurry vision, and floaters, and may lead to vision loss if not treated promptly.
Uveitis can be caused by autoimmune diseases (such as lupus or sarcoidosis), infections (like herpes or tuberculosis), trauma, or eye surgery. In many cases, no clear cause is identified—this is called idiopathic uveitis. Proper diagnosis is key to finding the underlying cause and guiding treatment.
Common symptoms include:
- Eye redness or pain
- Blurry vision
- Sensitivity to light (photophobia)
- Floaters or spots in your vision
Symptoms can come on suddenly or develop over time. If you experience any of these, it's important to get evaluated quickly to protect your sight.
Diagnosis starts with a comprehensive eye exam and review of your medical history. We may use imaging tools like OCT (optical coherence tomography), fluorescein angiography, or ultrasound to detect inflammation. Blood tests and systemic evaluations may be recommended if an autoimmune or infectious cause is suspected.
It can be. Some forms of uveitis are short-term and resolve with treatment, while others are chronic and require long-term management. Chronic uveitis can cause complications like cataracts, glaucoma, or macular edema. Regular monitoring and timely treatment adjustments are essential to protect your vision.
Treatment depends on the cause and location of inflammation. Options include:
- Corticosteroid eye drops
- Oral anti-inflammatory medications
- Steroid injections
- Immunosuppressive or biologic medications for autoimmune-related uveitis
- Surgery (in complex or recurrent cases)
We customize your treatment to control inflammation while minimizing side effects.
Yes. Uveitis is often associated with systemic conditions like rheumatoid arthritis, lupus, ankylosing spondylitis, sarcoidosis, or inflammatory bowel disease. We coordinate with your rheumatologist or primary care doctor when needed to manage your care holistically.
Yes—if left untreated, uveitis can lead to serious complications, including vision loss. But with early diagnosis, expert care, and proper follow-up, most patients can maintain good vision and prevent long-term damage.
You’ll receive:
- A thorough eye exam
- Specialized imaging to assess inflammation
- A discussion about potential causes
- A personalized treatment plan
Treatment often begins the same day. We’ll also schedule follow-up visits to track your progress and adjust medications as needed.
At CLS Health, your care is led by Dr. Sandip Suresh, a board-certified ophthalmologist with specialized fellowship training in uveitis, ocular immunology, and advanced cataract surgery. He trained at the prestigious UCLA/Jules Stein and OHSU/Casey Eye Institutes and brings deep expertise in diagnosing and treating even the most complex inflammatory eye conditions.


